A ventricular assist device is a mechanical heart pump that is inserted into your heart to help it distribute blood throughout your body. VADs are often used as short-term, temporary support while you wait for heart transplant. Thanks to advances in VAD technology, the devices are now smaller and more portable and are also used as a long-term treatment for people who aren’t candidates for a heart transplant. This is called a durable VAD, destination therapy, or chronic therapy, and it can add years to your life. Many people with VADs report noticeable improvements in heart failure symptoms like shortness of breath, swelling, and energy levels.
Parts of a VAD
VADs have four main parts.
- During open heart surgery, a small mechanical pump is attached to the left or right ventricle (the left is most common), the heart’s chamber that is responsible for most of the pumping action. The pump is also attached to the aorta, which is the main artery that delivers blood to the body. The attachment to the left ventricle is the reason these devices are often called left ventricular assist devices or LVADs.
- A thin tube called a driveline directs wires from the pump inside the body through a small hole in the abdomen. The wires are connected to a controller outside the body.
- The controller is a small computer (about the size of three stacked cell phones) that operates the pump and displays messages and alarms.
- Either batteries or a unit attached to an electrical outlet powers the device and is connected to the controller.
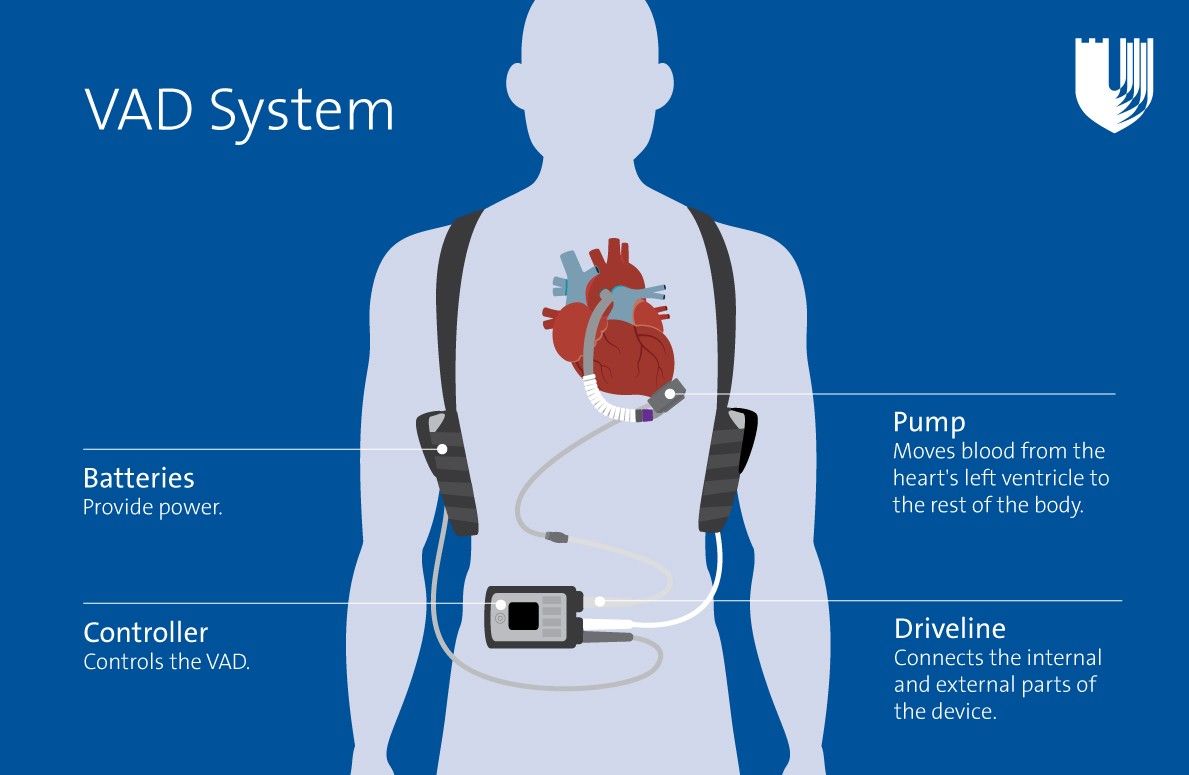
Parts of a VAD system include batteries that provide power, a pump that moves blood from the heart's left ventricle to the rest of the body, a controller that controls the VAD, and a driveline that connects the internal and external parts of the device.
Possible Complications
There are risks associated with VAD support, including hospital readmission, stroke, infection, and bleeding. If complications occur, you may need another surgery or a new VAD. Duke is dedicated to reducing your risk of these complications.
