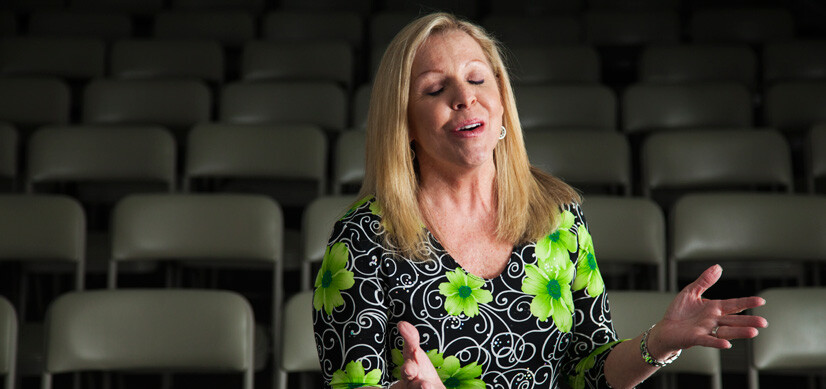
Helen Wadford sings the Duke team's praises for helping her beat stage 4 lung cancer.
Helen Wadford’s cancer survivorship story is so remarkable, it had become the stuff of legend. “I heard you gave one of your patients a pill and she sang at church that evening,” said a new lung cancer patient to Jennifer Garst, MD, lung cancer specialist and director of oncology clinical research at Duke Raleigh Hospital. The patient didn’t know Wadford personally, but knew her story.
Although Wadford’s triumph over cancer wasn’t quite that simple, it was dramatic enough to hearten those faced with the disease. In January 2012, the 56-year-old Louisburg, North Carolina, resident noticed a cough that she assumed was … a cough. Months later, the cough was still there, and she felt terrible. A CT scan confirmed the worst: stage 4 lung cancer.
Clearing the Air
For many people, hearing of a lung cancer diagnosis leads to the assumption that the patient is or was a smoker. Not true for Wadford—or for 15 to 18 percent of all lung cancer diagnoses. “This is not your grandfather’s lung cancer,” Garst says. “The percentage of people with lung cancer who have never smoked has been slowly growing over the past 10 years.” The alternate cause? For some, it is a genetic mutation.
The silver lining to a genetic mutation is that there are now two targeted drugs to treat these lung cancers. Targeted therapies can be very effective, with fewer side effects. “Chemotherapy is like a cluster bomb,” Garst explains. “It kills the cancer, but it kills healthy cells as well. Targeted therapies are like heat-seeking missiles. They attack the tumor cells directly and have fewer side effects.”
Of all lung cancers, nine percent will have a mutation that can be treated with a targeted therapy called erlotinib; five percent can be treated with one called crizotinib. “We routinely test all lung cancer specimens for specific genetic mutations,” Garst says. “If the mutation is present, targeted therapy is better than chemotherapy.”
What a Pill!
The thoroughness of Wadford’s first appointment with Garst took her by surprise. “I met with all the people on the lung cancer team,” she says. “They were remarkable, over the top.” Garst told her then that she wanted to test her for the genetic mutation.
Wadford tested positive and was treated with erlotinib. “When Dr. Garst came in to tell me I had tested positive, she was beaming,” Wadford says.
Instead of infusions, Wadford took a pill every day, beginning September 2012. She did not lose her hair, although it did thin. She developed a temporary rash on her chest and face.
By November, Wadford was in remission. She got this good news in the morning—that afternoon there was to be a benefit put together by her friends. Garst gave her prints of two X-rays of her lungs: the one from her first appointment and the current one. As she and her husband drove to the benefit, Wadford says, “I was about to bust open with the good news. My husband showed those X-rays around as if he was showing a newborn baby.”
And yes, she did sing at church—a solo—two days after the benefit. “And I’ve been singing ever since,” she says.
Lung Cancer Screening Saves Lives
Although Wadford was never considered at high risk for lung cancer before her diagnosis, there are guidelines that can identify those at high risk. For these people, the same test that was so important to Wadford’s diagnosis—the low-dose spiral computed tomography (CT) scan—can save lives.
“Usually the patients we see have self-identified as high risk, so there is a lot of anxiety,” Garst says. “We take a good history, do a thorough exam, and do pre-test and post-test counseling.”
The scan specifically targets the lung tissue, with a fraction of the radiation dedicated to the rest of the chest. “We can catch lung cancer in its earliest stage,” Garst says. “This test is a huge step forward.”
All lung cancer patients at Duke Health benefit from a multidisciplinary team of specialists, including a surgeon, a medical oncologist, a radiation oncologist, and a pulmonologist. At Duke Raleigh, patients are shepherded through the treatment process and given emotional support by a patient navigator who helps coordinate all appointments.
Wadford credits her faith and prayers for her recovery, sings the team’s praises, and calls Garst “humble, personable, remarkable.” She says she is grateful—not only that her life is back to normal, but also that her story has gotten out and is inspiring others.